Have you just been diagnosed with endometriosis?
Well, let me reassure you that you do not have to suffer. Whilst you may have been told that there is no cure, the good news is, it can be managed with an appropriate and tailored approach.
Excitingly, more evidence is emerging highlighting how nutrition and dietary management can help with symptoms and, even slow the progression of endometriosis growth.
Two key therapeutic approaches which are currently in the spotlight are the low FODMAP diet and an anti-inflammatory way of eating.
Before we dive into why they have been found to be beneficial for many, it is important to understand that every woman will respond differently. This is why it is crucial to seek professional guidance from a qualified dietitian before making any dietary changes.
The Low FODMAP Diet:
I am sure many of you reading this are familiar or have at least heard of FODMAPs. However, if you have not come across it before, FODMAPs is simply an acronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. A mouth full, I know!
Simply put, FODMAPs are a group of carbohydrates that are either indigestible or poorly absorbed by some people1. Generally speaking, these carbohydrates are not to be feared as they are found in a wide variety of nutritious foods including; fruits, vegetables, grains and cereals, dairy foods, legumes and nuts and seeds.
What are the effects of FODMAPs?
As these carbohydrates travel through the gastrointestinal tract, they draw excess fluid into the small intestine and are fermented by bacteria in the colon resulting in the production of gas1. In certain people, the build-up of fluid and gas can subsequently lead to the many symptoms of irritable bowel syndrome (IBS) including excessive flatulence, bloating, abdominal pain, constipation and/or diarrhoea1,2.
What exactly is the low FODMAP diet?
The low FODMAP diet is a 3-step dietary protocol created for the management of IBS symptoms3. Specifically, it is a type of elimination diet in that, certain high FODMAP foods are removed from one’s diet for a period of time in order to investigate and identify sensitivities to particular foods3.
The underlying goal of this elimination diet is to achieve a ‘clean canvas’, so to speak. This means that we want the patient’s symptoms to improve. Once symptoms have improved (or disappeared) and the patient starts to feel a lot better, the next step is to reintroduce or ‘challenge’ high FODMAP foods to see if they cause or exacerbate symptoms3,4.
Now you might be thinking, why do I need to challenge high FODMAP foods when I feel amazing without them? Can’t I just stay on the low FODMAP diet forever? Well, it is actually super important to reintroduce as many as possible in amounts you can tolerate as our gut bacteria love feasting on high FODMAP foods5. In fact, many FODMAPs behave as prebiotics and thus, have positive effects on our gut health5. Therefore, restricting them long term could negatively impact your gut health and subsequently, your overall health5,6. Not to mention, the low FODMAP diet is quite restrictive and socially isolating.
During the challenge period, we look at not only which foods might cause upsets, but also in what amounts. This is because sometimes, a small or infrequent amount of high FODMAP foods is tolerated however, when consumed in larger amounts or more frequently, one’s symptoms can exacerbate4,5.
Once all high FODMAP foods are challenged and intolerances and intolerance levels have been identified, qualified dietitian’s work with individuals to develop a tailored style of eating that is balanced and best suited to tolerances.
What does all this talk about FODMAPs have to do with endometriosis? Well, excitingly, there is increasing evidence showing the role this diet can have in endometriosis management2,7.
The link between IBS and endometriosis:
Due to inflammation, women with endometriosis tend to have an overactive immune system and as such, also experience a number of gut symptoms7. Some common symptoms include changes to bowel habits (i.e. constipation and/or diarrhoea), food sensitivities and intolerances, digestive pain and bloating7,8. Thus, it is not uncommon for women to initially or, later, be diagnosed with IBS. In fact, women with endometriosis are 2.5 times more likely to be diagnosed with IBS!8
Whilst the connection between endometriosis and IBS is currently unclear, there are a few proposed ideas throughout the literature.
Interestingly, people with IBS and women with endometriosis both experience visceral hypersensitivity2. This is when the abdominal area is particularly sensitive to stimuli (i.e. gas). Stimuli such as gas, can trigger nerve endings in the abdominal region to send pain signals up to the brain2. This is thought to intensify the pain experienced by some women with endometriosis. Thus, there is accumulating evidence suggesting that the low FODMAP diet could be an effective therapy for some women2,7,8.
Additionally, both conditions share the commonality of chronic low-grade inflammation which essentially, maintains these conditions7. Because of this, it is thought that there is a mutual promotion effect between IBS and endometriosis, meaning, one makes the other worse7.
So, if you have been diagnosed with endometriosis and are also experiencing IBS like symptoms, it may be worth following a tailored FODMAP protocol for a period of time to reduce the load of fermentable carbohydrates in your diet and, potentially slow the progression of endometriosis. In doing so, your dietitian can help you determine which fermentable carbohydrates and at what amounts, exacerbate your symptoms.
The Anti-inflammatory way of eating:
Although there is no universal anti-inflammatory diet or regime as such, there are specific components that can support an anti-inflammatory trajectory. Since women with endometriosis experience a state of chronic low-grade inflammation, dietary factors that reduce inflammation are thought to assist in managing symptoms and potentially slow endometrial growth – this is because endometrial cells require a pro-inflammatory environment to settle and proliferate9.
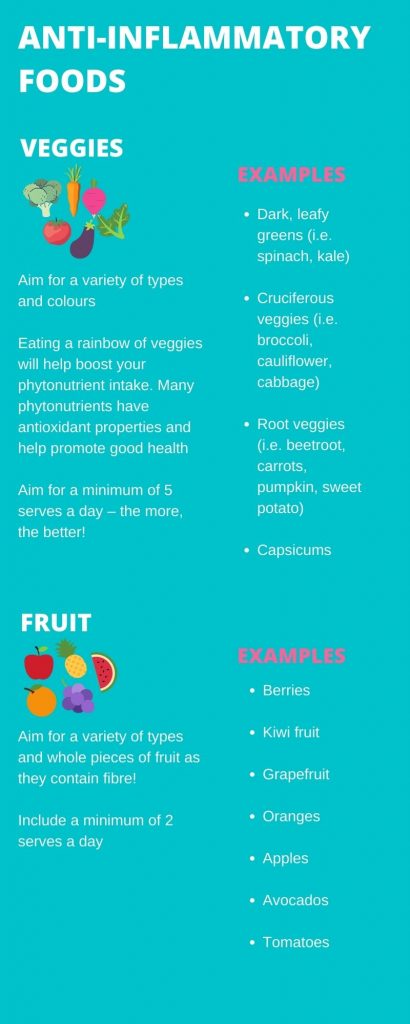
An anti-inflammatory diet or way of eating involves eating nutrient-rich wholefoods which contain plenty of fibre, antioxidants and omega-3 fatty acids. As such, this includes a diet abundant in vegetables, whole fruits, wholegrains, legumes and fatty fish9.
Dietary factors that can reduce inflammation:
Omega-3 fatty acids
Omega-3 fatty acids are known for their potent role in reducing inflammation and are found in a variety of foods including oily fish (i.e. salmon and trout), tofu, extra virgin olive oil and nuts and seeds (i.e. flaxseeds, chia seeds, walnuts).
The Australian Dietary Guidelines recommend we consume a balance of omega-3 and omega-6 fatty acids, as too much omega-6 can promote inflammation10. Concerningly, Australians tend to be consuming more omega-6’s relative to omega-3’s with an approximate ratio being 8:1 when the recommended ratio is 2:110. This indicates that most Australian’s are not consuming adequate amounts of anti-inflammatory omega-3’s.
Why are omega-3’s so important to consume if you have endometriosis?
Well, although evidence of the beneficial role of omega-3’s and endometriosis have come from a combination of human and animal studies, current evidence shows that sufficient intake of omega-3 fatty acids is associated with reduced inflammation and endometrial symptoms, such as pain11.
How? Studies have shown that omega-3 fatty acids seem to reduce inflammatory hormone-like substances called prostaglandins10,11. In some women suffering from endometriosis, prostaglandins are elevated in the abdominal fluid and as such, are thought to contribute to the pain experienced11,12.
How to add more omega-3s into your diet:
- Enjoy fish 2-3 x per week (try grilling, pan-frying or baking your fish)
- Sprinkle nuts and seeds on top of your main meals (good sources of Omega 3 being walnuts, chia, flax seed and hemp seeds)
- Include tofu a few times a week
Fibre
I am sure it comes as no surprise that consuming adequate fibre is essential for good health. However, this is especially true for women with endometriosis as fibre can help excrete excess oestrogen (via faeces)13. Excess oestrogen can be inflammatory and exacerbate endometriosis symptoms thus, consuming ~25g of fibre per day is important13,14. Consuming sufficient fibre can also assist in regular bowel movements which may help decrease bloating, pain and other IBS-like symptoms6. Fibre rich foods include veggies and fruit (bonus if you keep the skin on!), wholegrains, legumes and nuts and seeds.
How to ensure you are meeting your fibre requirements:
- Snack on fruits and veg (i.e. enjoy veggie sticks dipped in hummus)
- Grab a handful of mixed nuts and seeds as a snack
- Add more veggies to each main meal
- Swap to wholegrain breads and cereals
Antioxidants
Antioxidants have numerous roles and benefits in the body. When it comes to reducing inflammation, antioxidants neutralise the effects of free radicals in the body15. There are two classes of antioxidants; nutrient antioxidants and non-nutrient antioxidants. Nutrient antioxidants include vitamins A, C and E, and the minerals copper, selenium and zinc15. Non-nutrient antioxidants are simply other dietary food compounds which portray antioxidant properties such as phytonutrients – these are found abundantly in plant foods15.
How to increase your antioxidant intake:
- Add more veggies to each main meal
- Aim to consume 30 different plant foods across your week (this includes fruits, veggies, wholegrains, legumes and nuts and seeds) – colour and variety is key!
- Snack on fruits, veggies and nuts and seeds
Foods That May Negatively Affect Endometriosis
Although more research is needed to identify exactly which foods and lifestyle habits may worsen endometriosis, the following factors are currently known to have a link:
- High trans-fat intake: trans-fats are found in highly processed foods, fried foods and refined seed oils. Avoiding or limiting trans-fats is recommended as they induce an inflammatory response in the body9
- High-FODMAP intake: as mentioned earlier in this post, some women with endometriosis may experience exacerbated symptoms following a high-FODMAP diet2,7,8
- High GI and excess refined sugar intake: both increase insulin and inflammation in the body which may worsen endometriosis symptoms2
- Alcohol, caffeine, gluten and red meat have also been shown in some studies to promote inflammation in the body9. Therefore, it is recommended to limit your intake
- BPAs: whilst not a dietary factor, research indicates that excess exposure to BPAs may influence hormonal balance16. Since current research is limited, avoiding or at least limiting BPA exposure, may be beneficial for women with endometriosis
What about soy?
Many women with endometriosis ask if, or assume, they should avoid soy altogether due to its phytoestrogen content. However, you may be surprised to know that inclusion of soy foods (i.e. tofu, soy milk, edamame) in one’s diet has many benefits, including in women with endometriosis. Whilst there is currently insufficient evidence to indicate that soy can be harmful in women with endometriosis, like with all foods, balance is key. Therefore, it is not advised to consume soy in excess17.
What might excessive soy intake look like? It may look like; 1 x cup of soymilk with breakfast, soymilk in coffee/tea, tofu for lunch, and tempeh for dinner most days of the week. If concerned about your soy intake, it is best to reach out and consult with a dietitian.
Below is a link to an infographic outlining examples of anti-inflammatory rich foods. This is by no means an exhaustive list; however, I hope this will help provide you with a basic overview. As always, it is recommended you consult your dietitian before altering or changing your diet.
Key Takeaway
Whilst diet and nutrition are not the solution to endometriosis and should not be implemented in isolation, it is worth exploring these options with a qualified dietitian. In doing so, and in conjunction with other therapies (i.e. stress management, adequate sleep, gentle movement), it is possible to manage your symptoms and potentially slow the progression of endometriosis.
And one more thing, the image used above is of banana rice flake porridge which, if following a low fodmap diet and/or an anti-inflammatory way of eating, is one great start to the day. It’s particularly nice when topped with seeds, nuts, cinnamon and berries.
References
- Moore JS, Gibson PR, Perry RE, Burgell RE. Endometriosis in patients with irritable bowel syndrome: Specific symptomatic and demographic profile, and response to the low FODMAP diet. Aust N Z J Obstet Gynaecol. 2017;57(2):201-5.
- Issa B, Ormesher L, Whorwell PJ, Shah M, Hamdy S. Endometriosis and irritable bowel syndrome: a dilemma for the gynaecologist and gastroenterologist. Obstet Gynaecol. 2016;18(1):9-16.
- Massimo B, Sara T, Maria Gloria M, Francesco B, Andrea P, Lorenzo B, et al. Low fermentable oligo- di- and mono-saccharides and polyols (FODMAPS) or gluten free diet: What is best for irritable bowel syndrome? Nutrients. 2020;12(3368):3368-.
- Starting the Low FODMAP Diet – Monash Fodmap [Internet]. Monashfodmap.com. [cited 21 July 2021]. Available from: https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/
- Mansueto P, Seidita A, D’Alcamo A, Carroccio A. Role of FODMAPs in patients with irritable bowel syndrome. Nutr Clin Pract. 2015;30(5):665-82.
- Liu J, Chey WD, Haller E, Eswaran S. Low-FODMAP diet for irritable bowel syndrome: What we know and what we have yet to learn. Annu Rev Med. 2020;71:303-14.
- Viganò D, Zara F, Usai P. Irritable bowel syndrome and endometriosis: New insights for old diseases. Dig Liver Dis. 2018;50(3):213-9.
- Seaman HE, Ballard KD, Wright JT, de Vries CS. Endometriosis and its coexistence with irritable bowel syndrome and pelvic inflammatory disease: Findings from a national case-control study-Part 2. Bjog. 2008;115(11):1392-6.
- Gaibisso T. Is there a universal diet for Endometriosis? [Internet]. Endometriosis Australia. 2020 [cited 17 July 2021]. Available from: https://www.endometriosisaustralia.org/post/is-there-a-universal-diet-for-endometriosis
- Meyer BJ. Australians are not Meeting the Recommended intakes for omega-3 long chain polyunsaturated fatty acids: Results of an analysis from the 2011-2012 National Nutrition and Physical Activity Survey. Nutrients. 2016;8(3):111.
- Khanaki K, Nouri M, Ardekani AM, Ghassemzadeh A, Shahnazi V, Sadeghi MR, et al. Evaluation of the relationship between endometriosis and omega-3 and omega-6 polyunsaturated fatty acids. Iran Biomed J. 2012;16(1):38-43.
- Hidalgo M, Ratto M, Burgos R. Apolipoproteins, Triglycerides and Cholesterol. IntechOpen; 2020. DOI: 10.5772/intechopen.89351
- Chantalat E, Valera MC, Vaysse C, Noirrit E, Rusidze M, Weyl A, et al. Estrogen receptors and endometriosis. Int J Mol Sci. 2020;21(8).
- Fibre | Nutrition Australia [Internet]. Nutrition Australia. 2014 [cited 16 July 2021]. Available from: https://nutritionaustralia.org/fact-sheets/fibre/
- Antioxidants – Better Health Channel [Internet]. Betterhealth.vic.gov.au. 2020 [cited 16 July 2021]. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/antioxidants
- Ohore OE, Zhang S. Endocrine disrupting effects of bisphenol A exposure and recent advances on its removal by water treatment systems. A review. Sci Afr. 2019;5:e00135.
- Mumford SL, Weck J, Kannan K, Buck Louis GM. Urinary phytoestrogen concentrations are not associated with incident endometriosis in premenopausal women. J Nutr. 2017;147(2):227-34.
Written by Jasmine Genau
Jasmine is a student nutritionist and aspiring dietitian from Deakin University with a special interest in fertility health, pregnancy and paediatric nutrition, mental health, and sports nutrition. Upon completion of her masters, Jasmine aspires to work as a clinical dietitian and to initially upskill in the areas of paediatric and sports nutrition.